This is the second in a series of posts on groin pain. If you missed the case study on which this series is based, go back to Groin pain Part 1: The case of Enrique L.
When a patient comes to my Boston area office with groin pain, what do I think about as a Neuromuscular Therapist. There are six factors to consider therapeutically, and there are medical conditions that need to be ruled out. Check for disease of the hip joint, a bone fracture, inflammation of the disc at the pubic bone, joint misalignment, a swollen bursa and an inguinal hernia.
First I think about injury or spasm in the local muscles. If there is no “groin pull” injury like what athletes describe, sports injury such as skiing or horsebackriding, accident like slipping on ice or trying to avoid a fall, then it probably comes from sitting or crouching or sleeping in a position where the hip is flexed for prolonged periods of time. It’s not uncommon with construction workers who do a lot of work on or near the floor. Those who must drive or travel for hours, especially with the hips jackknifed with the knees higher than the butt can experience groin tension. Sleeping in a fetal position is often the cause.
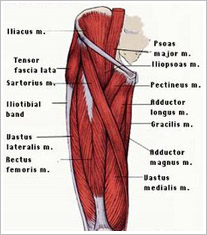
The second thing I think about is Trigger Points that refer pain to the groin. The most common are the long and short adductors, but pain can come from the iliopsoas and some of the hip flexors. There are no surprises here. Everything is pretty localized.
Next I think about possible entrapments of nerves or blood vessels. The femoral nerve and artery are right there in the femoral triangle at and below the crease in the thigh, but there are a total of five nerves in the area that can be involved.
The fourth NMT consideration is structural asymmetry. It isn’t known to cause problems in the three adductors, but the pectineus and any of the hip flexors can become overloaded by compensation caused by a short leg syndrome or uneven pelvis.
Fifth are systemic factors. Vitamin inadequacies, subclinical thyroid hypoactivity (underactive), circulatory disorders or anemia, infection, allergies and food sensitivities should all be checked as in any myofascial pain syndrome.
Last are emotional and physical stresses. Psychological stress can cause tension in any muscle, but a protective attitude toward the sensitive pelvic structures could be considered. Postural or positioning stresses that cause prolonged hip flexion may need to be modified or avoided such as sitting with the knees spread as in a lotus position or with the legs crossed, and any prolonged position with hip flexion.
The next post is Groin pain: The muscles simplified.